Background
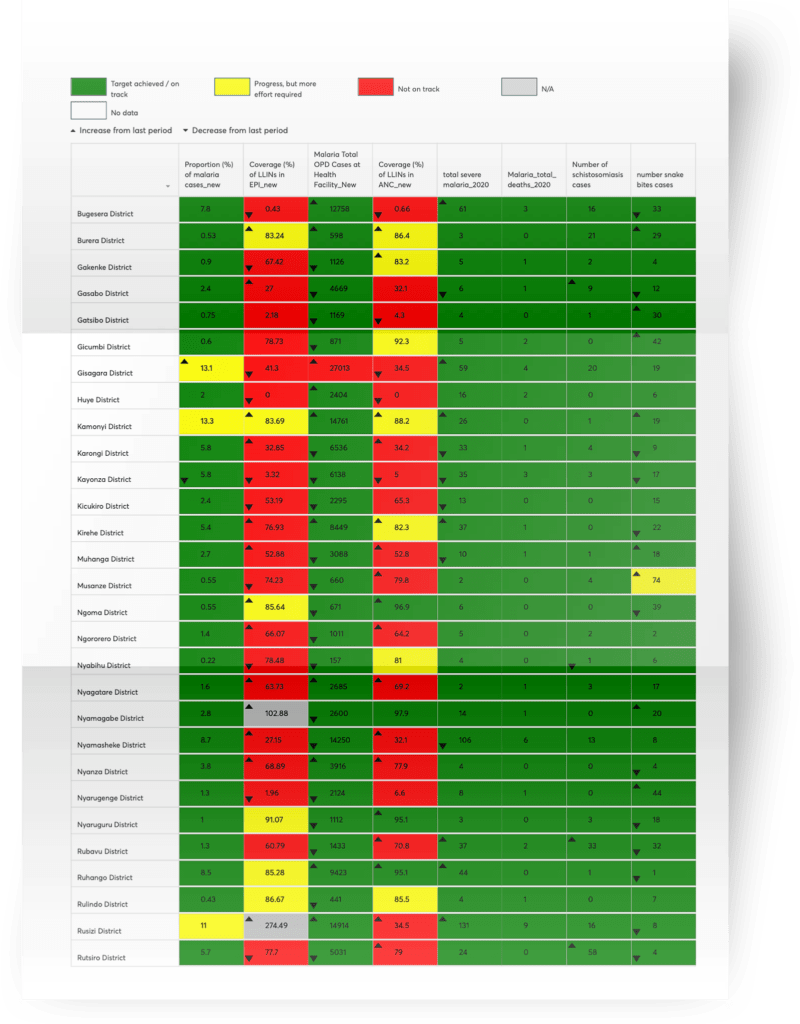
The Rwanda malaria scorecard was initiated with support from ALMA in October 2017 and tracks progress of indicators that reflect the priorities and objectives outlined in the Malaria Contingency Plan (MCP) 2016 to 2020 and the Extended National Strategic Plan 2016 to 2020.
How it works
The scorecard is produced directly in DHIS2 and discussed at several national level meetings including senior management meetings of the ministry of health and the Rwanda Biomedical Centre and at the sub-national level during district coordination meetings and health facility supervision meetings. In September 2020, a scorecard indicator review was conducted and a few priority NTD indicators were integrated into the malaria scorecard. In December 2020, the scorecard was decentralised, with all districts trained on the use of the tool to further enhance data-driven decision making.
Impact
Data quality
Close review of the data has led to the identification of how to improve the collection of data from community health workers and facilities to enhance data quality and adherence to national case management guidelines. As an example, an analysis of the scorecard by the National Malaria Control Programme seemed to show that health centres were using too many rapid diagnosis tests (RDTs) instead of blood smears. Consultation with health centres revealed that most of the RDTs were being used by health posts as recommended by the national guidelines. A recommended action was taken to separate health centres and health posts in the health management information system (HMIS) to correctly segment the data by type of facility to confirm compliance with guidelines.
Service delivery improvements
The scorecard is used for regular support supervision, allowing evidence-based supervision including follow up on areas of underperformance. For example, the scorecard has been used to address low coverage of long-lasting insecticidal nets (LLINs) through antenatal care. Technical staff followed up with health facilities and found that there was a stockout of LLINs for routine services that was not notified as LLINs were available for the mass campaign. The LLIN delivery was immediately triggered.
In a second example, it was found that some health centres were not complying with the guidelines for LLIN distribution. Staff were re-oriented. If the scorecard shows red on an indicator, which means the performance is not on track with the objectives set out in the strategic plan, this automatically triggers a supervision, which can also be online, through phone calls and emails, allowing for real time problem solving. In certain catchment areas, this has led to the timely identification of stockouts followed by the distribution of missing malaria commodities.
Key success factors
- Fully integrated within DHIS2
- Integration of both NTDs and Malaria Indicators
- Shared with partners
- Decentralised in all 30 districts of Rwanda
