Rwanda is one of the African countries that have shown tremendous progress toward the pre-elimination of malaria and control of neglected tropical diseases (NTDs). Efforts that have enabled this progress include innovative mechanisms such the deployment of community health workers to treat malaria, the use of drones for larviciding and the development of new accountability tools to track progress such as the malaria and NTDs scorecard. View the latest Rwanda malaria scorecard management tool.
Introduction: Malaria and NTDs in Rwanda
The Government of Rwanda has made tremendous progress towards the elimination of malaria and Neglected Tropical Diseases (NTDs) in Rwanda. Key interventions have included the increased coverage of Indoor Residual Spraying (IRS), the distribution of long-lasting insecticidal nets to the populations at risk, initiation of Home-Based Management (HBM) to test and promptly treat all suspected malaria cases in adults and children. Furthermore, effort has been put in place to establish community based integrated Vector Management (IVM) including outdoor control of mosquitoes through larviciding. These efforts have resulted in a reduction of the malaria incidence by 63% from 407 cases per 1000 in 2016 to almost 148 cases per 1000 in 2020, and a reduction in mortality by 79% from 706 deaths to 149 over the same period.
Since 2008, Malaria and NTDs control programmes are integrated in Rwanda and the vision of the Government of Rwanda is to be free from NTDs. In line with this, the Ministry of Health has intensified efforts for Mass Drug Administration (MDA), raised community awareness for preventive measures on NTDs and strengthened WASH and NTDs case management in all health facilities. These combined efforts have resulted in significant successes, for example, the national prevalence of intestinal worms decreased from 66% in 2008 to 45% in 2014.
To sustain these gains and progress even further, more efforts are needed. According to the Health Sector Strategic Plan (HSSP IV), Rwanda plans to reduce the malaria incidence from 308/1,000 to 122 cases/1,000 population and the mortality due to malaria by 40% by 2024.
Development and strengthening of Rwanda’s malaria and NTD scorecard tool
To support the country efforts in progressing towards malaria elimination, the Rwanda malaria scorecard management and accountability tool was first developed in October 2017 with support from ALMA. In September 2020, a scorecard indicator review was conducted and priority NTDs indicators were integrated into the malaria scorecard, making it the first integrated malaria/NTD scorecard on the continent.
In December 2020, the scorecard was decentralised, with all 30 districts trained on the use of the tool to further enhance data-driven decision-making.
In 2020, the malaria scorecard was also revised and adapted for use by the Civil Society Organisations (CSO).
Besides the malaria and NTDs scorecard, Rwanda is also implementing a Reproductive, Maternal, Neonatal, Child and Adolescent Health scorecard to track maternal and child health priority indicators. View the Rwanda RMNCAH scorecard.
Rwanda’s malaria and NTDs scorecard: an accountability tool that tracks progress towards health programme goals
How it works
The scorecard tracks performance of a set of high-priority malaria and NTD indicators selected to reflect progress towards NTD and malaria strategic plan goals. The scorecard is produced every quarter on DHIS-2. Data for the scorecard indicators are extracted from the existing health management information system (DHIS-2) as the primary source of data. In addition, the scorecard also pools data from other reporting systems such as the Logistics and Management Information System (LMIS), the Disease Surveillance Systems (Electronic Infectious Disease Surveillance and Response System or eIDSR) and ‘RapidSMS’, an mHealth system used by Community Health Workers (CHWs) across Rwanda. Through the DHIS-2 scorecard app, the scorecard is produced, and indicator performance displayed visually in colour codes. Before publication of the scorecard, the malaria and NTDs division at RBC conduct data quality checks. The scorecard is also published on the ALMA Scorecard Hub every quarter.
Indicators
The design and selection of indicators for Rwanda’s malaria and NTDs scorecard were based on the national priorities and targets set in the national strategic plan and aligned with the 5-year milestones in the World Health Organization (WHO) Global Technical Strategy for Malaria 2016 to 2030. The scorecard indicators focus on the thematic areas: malaria prevention, case management, disease burden and key policy issues for malaria control and NTDs.
Indicators currently include:
| Categories | Indicators |
| Case management | Malaria proportional morbidity OPD Annual parasite incidence per 1,000 persons Number of malaria cases (average cases) Number of severe malaria cases (average cases) Inpatient malaria death per 100,000 persons per year Number of malaria death per month (average cases) Percentage of persons treated within 24 hours from onset of symptoms at the community level |
| Prevention | Percentage of children under 1 year who receive LLINs through EPI (Measles and Rubella vaccination) Percentage of pregnant women attending first antenatal care visit who receive LLINs |
| NTDs | Number of schistosomiasis cases Number of snake bites cases reported |
Annually, the malaria and NTDs division at Rwanda Biomedical Centre (RBC) in close collaboration with partners and stakeholders, undertake a national consultative process to set national targets and thresholds (that define the red, yellow and green colour codes on the scorecard) for malaria and NTDs scorecard indicators. This process is undertaken in close coordination with the Malaria Technical Working Group—a national dialogue and coordination forum with government, partners, and stakeholders at the national level, which reviews and approves the scorecard colour code and targets.
District level targets
The national scorecard is also produced to show performance by district, and respective districts can be compared with each other. Every quarter, the district hospital managers produce the district malaria and NTDs scorecard through the DHIS-2 app.
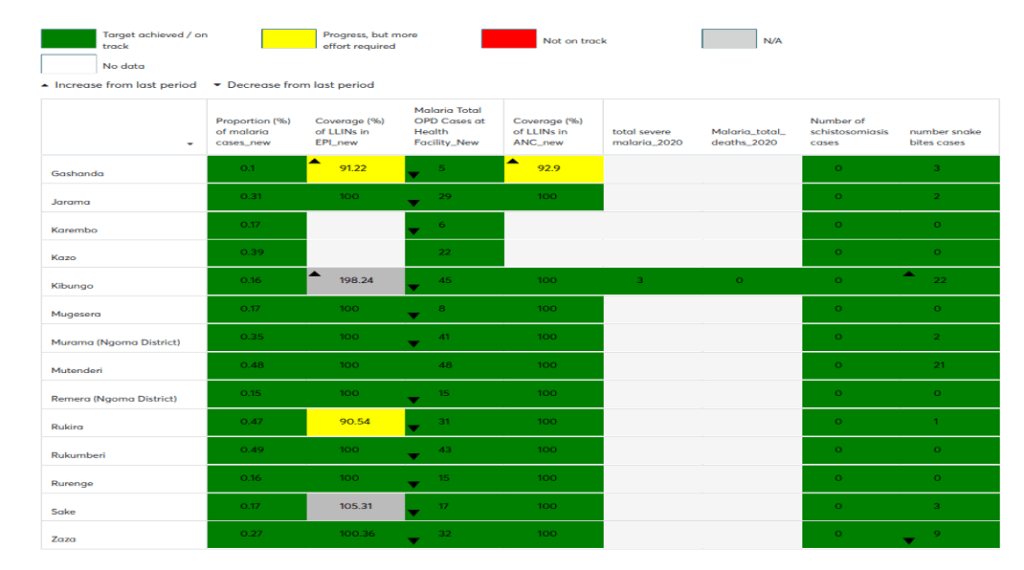
Source: Kibungo Hospital, Ngoma district Scorecard based on the DHIS-2, May 2021
Each of the 30 districts in Rwanda contextualises the national targets and develops district-specific performance targets. District targets are established in collaboration with the Malaria programme managers at RBC/MoH and through consultations overseen by the District Health Management Team (DHMT) –– a coordination forum of health actors at the district level. The district scorecard data can also be disaggregated to show performance by sector, cell, and village, and compare performance across the district and helps to drive action.
The analysis of the scorecard has helped us collectively analyse bottlenecks and take action.
Dr William Rutagengwa, Director General Nyamata Hospital in Bugesera District
Review of the scorecard during management meetings
The review of the scorecard is integrated into existing coordination forums at national and decentralised level.
At the national level, the review of the scorecard through the Malaria and NTDs Technical Working Groups (TWG), a coordination forum that reports directly to the Minister of Health, has been a key factor of success, as the Ministry’s leadership is directly involved and has visibility of the most recent data.
At the decentralised level, the implementation of the scorecard is coordinated through the district hospitals, health centres, district health unit, district health management team, with involvement of partners through the Joint Action Development Forum (JADF), District coordination meetings and the health facility supervision/Data Quality Audit (DQA) feedback meetings. Through these coordination forums, every quarter the district health actors review the scorecard, and this has resulted in the identification of bottlenecks and actions to address the problems in malaria elimination. Actions are taken and implemented by different levels of the health system and at the district, health centre and community level.
The use of a scorecard is a very important part of programme implementation. The National Technical Working Group uses this scorecard as a means to monitor and evaluate and be able to see programme performance at national level as well as at subnational level in the districts.
Dr Kasonde Mwinga, WHO Country Representative/Rwanda
Impact
The scorecard is used as a tool to monitor achievement of strategic goals improving data use, partner coordination, stakeholder accountability and action.
Enhanced partner coordination
The implementation of the scorecard stimulates stakeholder collaboration, coordination and accountability.
Every quarter after it is produced, central level teams analyse the scorecard, prioritize the areas requiring attention, and develop action plans to address emerging issues like the gaps in coverage of LLIN at health centres. The scorecard is then discussed at the Malaria and NTDs Technical Working Groups.
In addition, the scorecard is used to guide Malaria Programme and partner’s efforts to target interventions in districts with poor performance (Supervisions, Data Quality Assurance, malaria commodities redistribution).
As partners, the scorecard has been a helpful tool for partner coordination where we discuss progress on malaria priority indicators performance and hence facilitating real-time actions and follow up.
Manasseh GIhana Wandera – Executive Director, SFH Rwanda
Resource mobilisation
The malaria and NTDs scorecard, combined with wider data use, is a useful management tool to mobilise resources and appropriately allocate resources.
As an example, the scorecard review in 2019 identified 12 high malaria prevalent districts and actions were undertaken to intensify IRS in these districts. Using the Scorecard and Programme Data, the Government of Rwanda secured additional funds (approximately USD 2.5 Million) to increase and sustain IRS in 5 districts and introduce New Generation LLINs in 9 Districts with documented mosquito insecticide resistance.
The scorecard easily convinces our partners on resources needed to move from red colour (indicators lagging) to green colour (indicators on track) for some indicators.
Honourable Tharcisse Mpunga, MD, MSc – Honourable State Minister of Health, Government of Rwanda
Improved data quality and enhanced use of data for decision making
The scorecard is an important resource for enhancing the use of data for greater transparency, accountability and evidence-based decision making.
For example, an analysis of the scorecard by the malaria and NTDs division revealed that health centres were using too many rapid diagnostic tests (RDTs) instead of blood smears. Consultation with health centres revealed that most of the RDTs were being used by health posts as recommended by the national guidelines. A recommended action was taken to separate reporting for health centres and health posts in the health management information system to correctly segment the data by type of facility to confirm compliance with guidelines.
Implementation of the scorecard has greatly revolutionized DHIS-2 data use and improved data quality on Malaria indicators across the health sector. The colour codes are easy to identify that something is wrong, and then we immediately do a follow up. In most cases we have identified data quality issues that are immediately rectified.
Dr Aimable Mbituyumuremyi, Division Manager Malaria and NTD’s, MoH/RBC
Evidence based supervisions
The scorecard is used for regular support supervision, allowing evidence-based supervision including follow up on areas of underperformance. If the scorecard shows red on indicators such as ‘Percentage of persons treated within the 24 hours from onset of symptoms at the community level’, this triggers supervision, which can also be ‘online’, through phone calls and emails, so does not have to wait months until next supervision to fix the problem. For example, the scorecard has been used to address low coverage of long-lasting insecticidal nets (LLINs) through antenatal care. Technical staff followed up with health facilities and found that there was a stockout of LLINs for routine services that was not reported as LLINs were available for the mass campaign. The LLIN delivery was immediately triggered. This level of review, quantification and redistribution has been instrumental in reducing stockouts.
Using the scorecard for home-based management helps us to focus target supervision by different partners and control in the central level to increase coverage or access and for us to achieve targets.
Honourable Tharcisse Mpunga, MD, MSc – Honourable State Minister of Health, Government of Rwanda
Service delivery improvements
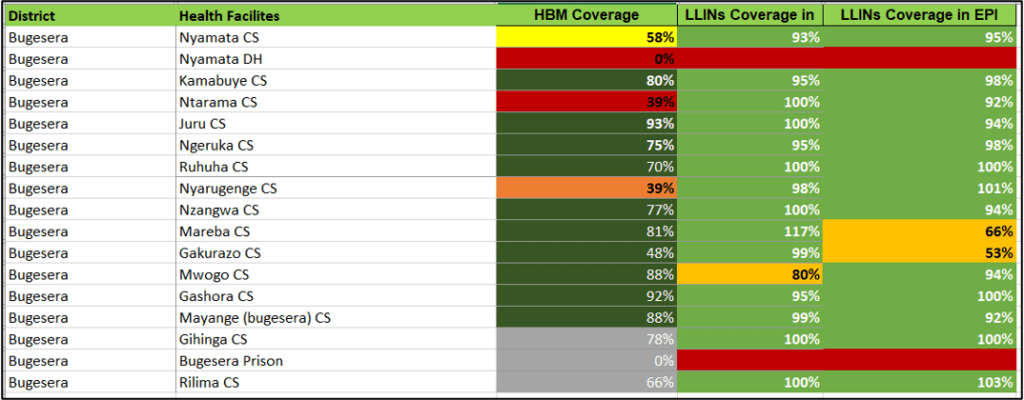
The review of the Q4 2020 scorecard revealed that Bugesera is among districts reporting schistosomiasis cases 9 times higher than the national average of 7 cases. A follow-up bottleneck analysis revealed the most prevalent areas in the district are those localized around bodies of water where freshwater snails live, which act as vectors for the disease. Actions were taken to increase coverage of preventative chemotherapy in Bugesera district.
Key success factors
Leadership commitment
The involvement of top Ministry of Health leadership has greatly contributed to the success of scorecard implementation. Top leadership is using the scorecard leading to action and high level awareness of health bottlenecks.
Decentralisation
The decentralisation of malaria and NTD scorecard has been another great achievement In Rwanda. Currently, all 30 districts are able use the scorecard and it allows to tailor performance monitoring and enhance decentralised decision-making and action by setting realistic and achievable targets for each district.
Integration into the DHIS2 system
The malaria and NTDs scorecard has been fully integrated within the existing health management information system (DHIS2), which is the primary source of data for populating and producing the scorecard. This has been particularly important in institutionalising scorecard implementation. The scorecard is now produced from routine data collected in DHIS2, a platform that most health sector managers even those at the decentralised level are very much familiar with.
We are familiar with DHIS2 in reporting health related activities monthly. The use of the Scorecard has helped us use the data that we report, evaluate the quality and facilitating real-time actions and follow up.
Dr William Rutagengwa, DG Nyamata Hospital
Integration of the scorecard review in existing accountability mechanisms
The implementation of the malaria and NTD scorecard has been integrated within the existing coordination structures and forums at the national and decentralised level. This involves priority indicator setting, setting national and district respective targets, production, and analysis. The process is participatory and has been coordinated through the existing coordination forums at the central and decentralised level. This has been very instrumental in ensuring the institutionalisation of the scorecard in Rwanda.
Success story: Using scorecard data for improving efficiency of existing malaria resources in Ngoma District
Introduction: Ngoma, a high-endemic district located in Rwanda’s Eastern Province
Ngoma district, located in Rwanda’s Eastern Province, is among the country’s 12 high malaria endemic districts. The implementation of Indoor Residual Spraying (IRS) in 2018 led to a significant decline in malaria incidence from 1469 cases per 1000 population in 2018 to 649 cases per 1000 in FY 2019.
Despite these efforts, the district still accounts for a high malaria burden. Within the district itself endemicity is not equally distributed, and malaria vulnerability is not evenly distributed across all health centre catchment areas. Therefore district leaders needed a way to access timely information on the malaria burden for each specific health centre for targeted intervention deployment.
Actions taken as a result of the analysis of the district’s first scorecard
In March 2021, the Kibungo Hospital in Ngoma district produced the first malaria and NTDs scorecard and showed the status of malaria burden in different health centres within its catchment area. The district health unit presented the scorecard in the Joint Action Development Forum (JADF) meeting and actions were taken.
The scorecard revealed that some health centre catchment population had more than 100 cases/1000 population while some had zero cases. It showed that cases of malaria in March 2021 reduced in Kibungo, Mutenderi and Gashanda health centrescompared to January 2021 but inversely, the cases increased tremendously in Jarama, Remera Ngoma and Nyange Health Centers in March compared to January 2021. Further analysis showed that there were stock-outs of LLINs and of Rapid Diagnostic Test kits. A decision was promptly made to reallocate commodities from the health centres with low cases to those with higher ones while waiting for the central level to send those commodities. Furthermore, the District Health Unit also commended health centres with lower cases to share their medicine stocks with those with higher burden and avoid that these medicines expire.
The malaria and NTD district scorecard is a great tool to reduce even the cost of medicine in the district or at a specific health centre as it can help to avoid loss of medicine and other commodities. The scorecard will now be discussed during all meetings that concerns health in Ngoma District.
Madam Kirenga Providence, Vice Mayor in Charge of Social Affaires, Ngoma district
Next steps
The pilot programme is on-going but initial use of the scorecard has showed its importance in informing prompt decision making. As of August 2021, all Director General of Hospitals have been trained and the scorecard is used routinely to prompt decision and increase accountability.
The analysis of the Malaria scorecard has changed the way data were analysed and considered. Previously, the district was looked as a whole, but currently the District Health Management Team and JADF concentrate their analysis to specific areas of the district, health centres where there are some problems and issues. In this regard, bottlenecks are defined and proposed solutions are provided to address these issues. Furthermore, the scorecard revives our regular coordination meetings as we have corrective actions to be implemented in the next upcoming quarter.
Madam Annick Mizero, Head of Health Centre Remera Kibungo, Ngoma district
Innovation in the use of the scorecard tool: Piloting the CSO adapted scorecard
Background
Using a grant from the Global Fund to strengthen social behaviour change communication (SBCC) for malaria countrywide, five civil society organisations (CSOs) including CARITAS -Rwanda, RICH, SFH Rwanda, Profemme Twese Hamwe and URUNANA DC were contracted to support SBCC interventions aimed to fight malaria in the community.
The Civil Society Organisations (CSOs) started supporting the Malaria program in January 2021.
Initial steps involved:
- stakeholder consultations through the malaria Technical Working Group
- identification of priority malaria indicators for the CSO adapted scorecard
- defining baseline and targets depending on malaria burden
Indicators for the CSO adapted scorecard
The CSOs adapted scorecard indicators are similar to the Malaria and NTDs indicators and adapted to focus on implementation at health centre and community level from a behaviour change communication perspective.
Currently, the CSO adapted scorecard has 3 indicators including:
- Proportion of Malaria Cases Diagnosed and Treated by Community Health Workers (CHWs)
- Coverage of LLINs in Antenatal Care Services for pregnant women
- Proportion of LLINs in Vaccination Programme for Under 1 Year
How it works
The scorecard used by the CSOs is produced through the DHIS-2 every quarter. Malaria and NTDs division is responsible for production of the scorecards for each district and sharing them with the five CSOs.
Through the coordination forums at the districts, the CSO discuss the scorecard with the decentralised level actors including the CSO staff allocated to the respective districts. In addition, the CSO discuss the scorecard with the community health workers and other community actors including cell and village administrative leaders. Bottlenecks are analysed and collective action is taken. The scorecard among other things has improved data use and been a useful tool to highlight priority areas for increased efforts and targeted interventions.
Using information from the CSO adapted scorecard, URUNANA DC organizes community trainings or provide prompt supervision and mentorship to CHWs workers for assuring the quality of the data reported, also make prompts advocacy to the Malaria Division in availing commodities or develop strategies to address issues reported.
Mr Gahenda Kasajja George, Executive Director, URUNANA D.C
Impact
Although the project only started in 2021, the malaria and NTD CSO adapted Scorecard is already proven to be a very useful tool to increase accountability and accelerate progress.
Enhanced community engagement
The CSO scorecard provides valuable information on the malaria burden in the community. Where a village shows a high number of cases, the community is directly involved in problem solving to increase prevention activities, for example encouraging households to sleep in the impregnated nets or eliminating stagnant water. For instance, in Gasabo district, communities were trained and informed on environmental management for malaria prevention.
Rapid action
The CSO scorecard can detect bottlenecks such as malaria or NTD commodity (LLINs, Rapid Diagnostic Tests, medicines) stockouts in the community. With this mechanism, the field officer can quickly escalate the issue without cumbersome processes.
