Introduction
Beginning in January 2018, the CSC was developed to enhance the health sector’s ability to gather public feedback on a quarterly basis on the delivery of health services. From the start, the CSC tool was integrated into Ghana’s Community-based Health Planning and Services (CHPS) program, a national strategy aimed at delivering essential community-based health services with the active involvement of communities. With extensive partner participation and media coverage during its development, the CSC is already receiving high visibility and recognition in the country. As of December 2019, impressive progress had been made with 11 regions out of the total 16 in the country participating in the CSC roll-out. Out of all 6,000 functional CHPS zones across Ghana, over 1500 (about 25%) have been trained on the CSC. This involved considerable partner support, particularly from WHO, USAID, the World Bank, the Doris Duke Charitable Foundation (DDCF) and ALMA. Most of the trained CHPS zones are also reporting data into DHIMS2 and a scorecard web platform that has the capacity to not only show real-time scoring data but also actions taken in response to the quarterly action plans
CSC operational steps
On a quarterly basis, the CSC tool and associated community-engagement processes (discussion, scoring, action planning and monitoring) are implemented at the community level. This includes four distinct steps completed by those with the following key responsibilities.

Key roles of stakeholders in CSC implementation
- Step 1 – CSC indicator discussion and scoring: CHMC (community health management committee), community
- Step 2 – Action planning: CHMC, community leaders, CHOs, facility head
- Step 3 – Action implementation: Community, CHMC, CHPS staff, SDHMT, DHMT
- Step 4 – Reporting CSC scorecard and updating actions planned and implemented: CHOs, district health information officers, action owners
Step 1: CSC Indicator Discussion and Scoring
Ghana’s Community Scorecard rating process involves three components:
- Preparation
- Scoring
- Ratings aggregation
Preparation
Preparation includes steps to be taken prior to conducting the community scorecard discussions. CHMC members invite relevant district and sub-district health management teams (HMTs) to the meeting; ensure needed materials are available (i.e. data collection sheets, calculator, pens); and arrange a facility tour for the CHMCs on the day of scoring to allow them to observe actions taken since the last quarterly meeting and gaps remaining. These tasks are generally performed by the Chairman of the CHMC and the CHO at the CHPS compound.
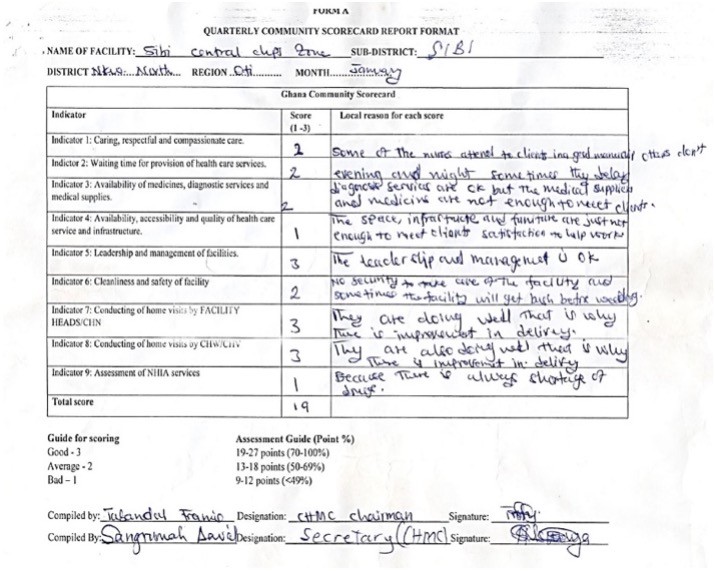
Scoring
Scoring of the quality of local health services based on the community’s experience and perceptions. This involves both group discussion and scoring based on the 9 indicators in the Scorecard. The meeting facilitator, typically the CHMC Chair, asks participants to consider and discuss for 5-10 minutes their health service experiences for each indicator and rate each indicator on a 1 – 3 scale.

Ratings aggregation
Ratings aggregation is done before the meeting concludes using the data collection sheet This allows for transparency before the final scores are disseminated or used to prepare the next quarter’s CHAPs (action plan). Final scores reflect either a majority score or a group consensus for each indicator and when aggregated reflect an overall composite average rating for each CHPS facility.
Important guidance includes
- Ideally 20-30 community members (including all CHMC members) should participate. Participants are to rate their specific facility (CHPS compound, health center or local hospital) on each of the 9 indicators using a scale of 1-3 (1 – Poor, 2 – Average, 3 – Good).
- Prior to voting, each indicator is to be discussed for 5-10 minutes.
- The score with the most votes is the score recorded on the provided scoresheet. In the case of a draw, the indicator definitions are discussed again and a consensus is reached through conversation.
- The CHPS/Facility staff, Sub-District Health Management Team (SDHMT) and District Health Management Team (DHMT) staff – as well as Regional Health Directorate (RHD) officers who may be supporting the process – do not participate in the scoring and are asked to also not be present at that time. These staff rather are present to respond to questions; clarify; and help in the action planning phase of the meeting.
- The meeting should conclude with a decision on the timing of the next quarterly meeting and a reminder that scorecard ratings and related agreed actions will be available on online for further review for all those with web platform accounts.
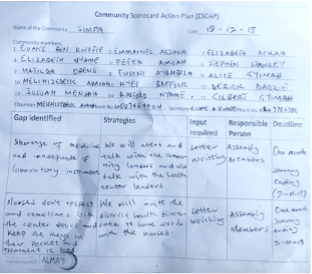
Step 2: Action plan development and dissemination
Community Scorecard data are then used by CHMCs, with CHPS staff in a supportive role, to develop a quarterly Community Health Action Plan (CHAP) – also known as a Community Scorecard Action Plan (CSAP).
A recent evaluation found that in those CHPS zones utilizing the CSC tool for production of Action Plans, there was enhanced collaboration between a range of stakeholders of the community health system (CHMC members, CHPS-level staff and volunteers, Facility In-Charges, District GHS staff, Chiefs and other Community Leaders). The CSC enabled the provision of technical support and funding from key partners such as WHO, the World Bank and USAID/Systems for Health to implement pragmatic action plans with timelines and specific roles assigned to committee members. Partners also appreciate that the CHAPs are also now public documents accessible to all stakeholders with access to the digital platforms. Additional partners have played various technical and other support roles at decentralized levels (e.g. UNICEF, UNFPA, the Institute for Healthcare Improvement’s UBORA Project, the National Program for Strengthening the Implementation of CHPS Initiative in Ghana (CHPS+), etc.).
Step 3: Action follow-up and implementation
With electronic alerts sent to action owners and their supervisors, including the Chair of the CHMC, via mobile phone and/or email, action implementation is followed by a number of stakeholders.
At the CHPS Zonal-level, actions are most often assigned to CHMC members and CHPS staff (CHOs, CHNs, CHVs) while at facilities the Facility-in-Charges are most often action owners. Quality Improvement Teams also follow-up on action implementation and when an action is beyond the community’s or facility’s capacity to undertake, the QI Teams bring it to the attention of the relevant Metropolitan, Municipal and/or District Health Management Teams for action.
Examples of action
Results from use of the CSC in Ghana are beginning to be documented.
Community empowerment and action
The CSC is widely credited with increasing community engagement and action to improve local health and well-being. Use of the CSC is leading to greater community involvement and local contributions thereby reducing the burden of health system management on the government. Examples include: (i) security improvements; (ii) donations of furniture to make client experiences more positive; and (iii) improvement of waste management and building maintenance.
Systems strengthening
The CSC tool is seen by the MoH as a catalyst in strengthening, and in some cases reactivating, regular discussion and action within CHPS zones around local health issues. Essentially the CSC has become the core implementation pillar of the CHPS strategy in those locations where it has been introduced. At the district and municipal levels, CSC scores were also beginning to be discussed at routine quarterly performance review meetings.
Service delivery improvements
In Ghana, the CSC has been described as a key ‘comprehensive performance assessment and planning instrument for service improvement’. Examples of service improvements in just over a year since training began include: (i) improvement in regularity and comprehensiveness of CHV home visits and (ii) reduction of stock-outs of essential drugs and supplies in health facilities.
We used to have our action plans in our offices so that only we can look at them but now it’s in the open for everybody to see so that anybody who walks in knows these are our challenges and this is what we are doing to improve on it
CHO-Adenkrebi CHPS, Ga East Municipal Health Directorate, GHS, Greater Accra Region
